What is Achilles Tendonitis?
 Achilles tendinosis is a soreness and stiffness that comes on gradually and continues to worsen until treated. It often starts with stiffness and creaking when first getting out of bed in the morning. Lightly pinching the Achilles tendon with the forefinger and thumb will indicate soreness. Achilles tendinosis is a common injury among middle and long distance runners. Achilles tendon rupture is a partial or complete tear of the Achilles tendon. It comes on suddenly, sometimes with a popping sound, and is debilitating. Partial and full Achilles tendon ruptures are most likely to occur in sports requiring sudden eccentric stretching, such as sprinting and racquet sports. Partial Achilles tendon tears are also common among middle and long distance runners. Achilles tendon ruptures are most likely to occur to middle age athletes who have not been training or who have been doing relatively little training. It is sometimes difficult to distinguish between Achilles tendinosis and a partial Achilles tendon tear. Consult a physician to be sure.
Achilles tendinosis is a soreness and stiffness that comes on gradually and continues to worsen until treated. It often starts with stiffness and creaking when first getting out of bed in the morning. Lightly pinching the Achilles tendon with the forefinger and thumb will indicate soreness. Achilles tendinosis is a common injury among middle and long distance runners. Achilles tendon rupture is a partial or complete tear of the Achilles tendon. It comes on suddenly, sometimes with a popping sound, and is debilitating. Partial and full Achilles tendon ruptures are most likely to occur in sports requiring sudden eccentric stretching, such as sprinting and racquet sports. Partial Achilles tendon tears are also common among middle and long distance runners. Achilles tendon ruptures are most likely to occur to middle age athletes who have not been training or who have been doing relatively little training. It is sometimes difficult to distinguish between Achilles tendinosis and a partial Achilles tendon tear. Consult a physician to be sure.
What Causes Injury to the Achilles Tendon?
There are several factors that can contribute to achilles tendonitis. First, you should know that the biggest contributor to chronic achilles tendonitis is ignoring pain in your achilles tendon and running through the pain of early achilles tendonitis. If your achilles tendon is getting sore it is time to pay attention to it, immediately.
Sudden increases in training can contribute to achilles tendonitis. Excessive hill running or a sudden addition of hills and speed work can also contribute to this problem. Two sole construction flaws can also aggravate achilles tendonitis. The first is a sole that is too stiff, especially at the ball of the foot. (In case you are having difficulty locating the “ball” of your foot, I mean the part where the toes join the foot and at which the foot bends) If this area is stiff than the “lever arm” of the foot is longer and the achilles tendon will be under increased tension and the calf muscles must work harder to lift the heel off the ground.
The second contributing shoe design factor which may lead to continuing achilles tendon problem is excessive heel cushioning. Air filled heels, while supposedly are now more resistant to deformation and leaks are not good for a sore achilles tendon. The reason for this is quite simple. If you are wearing a shoe that is designed to give great heel shock absorption what frequently happens is that after heel contact, the heel continues to sink lower while the shoe is absorbing the shock. This further stretches the achilles tendon, at a time when the leg and body are moving forward over the foot. Change your shoes to one without this feature.
Of course another major factor is excessive tightness of the posterior leg muscles, the calf muscles and the hamstrings may contribute to prolonged achilles tendonitis. Gentle calf stretching should be performed preventatively. During a bout of acute achilles tendonitis, however, overly exuberant stretching should not be performed.
Preventing Injuries to the Achilles Tendon
The best way to prevent an Achilles tendon injury is to a) stay in overall good shape, and b) warm-up, stretch, and strengthen the Achilles tendons. The best way to prevent an Achilles tendon injury from getting worse is to address the injury immediately: it will get worse if not addressed.
Treatment of Achilles Tendonitis
The first thing to do is to cut back your training. If you are working out twice a day, change to once a day and take one or two days off per week. If you are working out every day cut back to every other day and decrease your mileage. Training modification is essential to treatment of this potentially long lasting problem. You should also cut back on hill work and speed work. Post running ice may also help. Be sure to avoid excessive stretching. The first phase of healing should be accompanied by relative rest, which doesn’t necessarily mean stopping running, but as I am emphasizing, a cut back in training. If this does not help quickly, consider the use of a 1/4 inch heel lift can also help. Do not start worrying if you will become dependent on this, concentrate on getting rid of the pain. Don’t walk barefoot around your house, avoid excessively flat shoes, such as “sneakers”, tennis shoes, cross trainers, etc.
In office treatment would initially consist of the use of the physical therapy modalities of electrical stimulation, (HVGS, high voltage galvanic stimulation), and ultrasound. Your sports medicine physician should also carefully check your shoes. A heel lift can also be used and control of excessive pronation by taping can also be incorporated into a program of achilles tendonitis rehabilitation therapy. Orthotics with a small heel lift are often helpful.
Achilles Tendon Ruptures
The achilles tendon is the connection between the heel and the most powerful muscle group in the body. This has long been known as a site prone to disabling injury. It is named after Achilles, who according to myth was protected from wounds by being dipped in a magical pond by his mother. She held him by the heel, which was not immersed, and later died by an arrow wound in his heel. Although obviously, injuries to this area must have been known for more than 2,000 years, it was first reported in the medical literature by Ambroise Paré only 400 years ago.
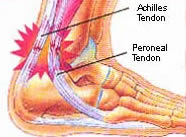
The achilles tendon joins three muscles: the two heads of the gastrocnemius and the soleus. The gastrocnemius heads arise from the posterior portions of the femoral condyles. The soleus arises from the posterior aspect of the tibia and fibula.
The gastrocnemius is a muscle that crosses three joints: the knee, the ankle, and the subtalar joint. The functioning of these joints and influence of other muscles on these joints has a significant effect on the tension that occurs within the achilles tendon. As an example tight hamstrings impact the functioning of the ankle joint, the subtalar joint, and increase tension in the achilles tendon. The soleus does not cross the knee and is a biarticualar muscle.
The plantaris is a nearby muscle that has its separate tendon. It arises from the lateral condyle of the femur. It has a thin tendon that passes between the gastrocnemius and soleus and inserts into the calcaneus. When this musclculotendinous structure is injured it is frequently felt as a “pellet shot” in the back of the leg. The tear is usually about eight inches below the knee joint.
The bulk of the achilles tendon inserts into the posterior superior third of the calcaneus. Some fibers course distally and continue to where portions of the plantar fascia insert into the plantar aspect of the calcaneus.
The achilles tendon does not have a rich blood supply. It is not invested within a true tendon sheath. A paratenon composed of other soft tissue surround it. The outer layer is a portion of the deep fascia, the middle layer is called the mesotenon and the inner layer is a thin layer. The blood supply to the proximal portion of the tendon comes from the branches of the muscles themselves. The distal portion is supplied by branches from the tendon-bone interface. The mesotenon supplies the major blood supply to the Achilles tendon.
The actual cause of rupture of the Achilles tendon is not known. The mechanism of injury is a force that increases the tensile force in the tendon beyond its tensile strength. This may be visualized as a dorsiflexion force at the foot or concomitantly a forward motion of the tibia over the foot while the calf muscles are contracting. As stated the force must exceed the tensile strength of the tendon. A forceful stretch of the tendon or a contraction of the muscles may create this force. Most often it is a combination of the two forces. Many researchers feel that some degeneration is present in the tendon prior to rupture. The usual site of rupture is approximately 2 to 6 centimeters proximal to the insertion in the calcaneus. This is also the portion of the tendon that has the poorest blood supply. Occasionally ruptures occur at the tendon-bone interface or musculo-tendinous junction. Since vascularity decreases with age, this frequently occurs in the ageing athlete. A weakening of the Achilles tendon has been observed following intra- tendinous steroid injection. Therefore, injections of steroids are not recommended at this location. Diseases associated with a possibly increased incidence of tendon rupture include gout, systemic lupus erythematosis, rheumatoid arthritis and tuberculosis.
Treatment for a Ruptured Achilles Tendon
Complete tears of the Achilles tendon, in the athlete, are usually treated with surgical repair followed with up to 12 weeks in a series of casts. Partial tears are sometimes treated with casting for up to 12 weeks alone, and sometimes are treated as are the complete tears, with surgery and casting. A heel lift is usually used for 6 months to one year following removal of the cast. Rehabilitation to regain flexibility and then to regain muscle strength are also instituted following removal of the cast.
